-
The Mind-Body Connection
Embracing an active lifestyle not only benefits our physical health but also nurtures our mental acuity, leading to a higher quality of life as we age. Dr. Zvinka Z. Zlatar highlights the potential benefits of physical activity in reducing the risk of Alzheimer’s disease and other cognitive issues. In her insightful presentation, she sheds light […]
-
Breastfeeding: Common Questions

Breastfeeding is a natural and beautiful way to nourish your baby. It can also be challenging and overwhelming for new mothers. Join Nancy White, RN, IBCLC, a board-certified lactation consultant, and Julia Cormano, MD, FACOG as they discuss the basics of breastfeeding, and provide helpful tips for your breastfeeding journey. Some of the questions they […]
-
Low Back Pain: What You and Your Doctor Should Know

It is estimated that more than 80% of adults in the U.S. will have low back pain at some time in their lives. It is a significant cause of disability, resulting in an immeasurable toll on function, happiness, and quality of life. This new series from UC San Francisco looks at what causes back pain […]
-
The Impact of Group Prenatal Care

“It instilled a lot of confidence in us going into labor and allowed us to be advocates for ourselves because we knew so much information going in – whether it was the doula program or where your baby was or just being familiar with the people around you. I felt very empowered going into my […]
-
Looking to a Future Without Alzheimer’s
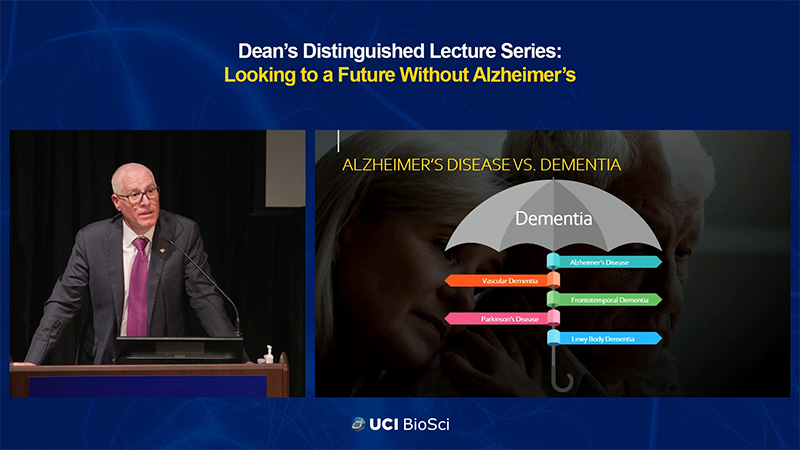
Alzheimer’s disease is a major health crisis that is projected to become an even larger threat in the coming decades. According to the National Institute on Aging, the number of Americans 65 and older with Alzheimer’s could rise from 5.8 million in 2020 to 13.8 million by 2050. Given the severity of this health crisis […]
-
Heart Health: Advances in Preventing and Treating Heart Disease

Delivered by world-renowned experts from the UCSF Health Division of Cardiology, this new series provides insights into advances in cardiology including the role of genetics, diet, exercise, and cholesterol in preventing and treating diseases of the heart. You’ll learn about advances in the prevention and treatment of coronary artery disease and heart attacks, abnormal rhythms […]
-
Confronting the Mental Health Crisis

Society continues to grapple with the challenges that people with mental health issues face. According to the Centers for Disease Control and Prevention, one in five Americans experience mental health problems. There are many factors contributing to our society’s struggle with mental illness. The lingering uncertainties of the COVID-19 pandemic, the ongoing conflict between Ukraine […]
-
International Efforts to Achieve Healthy Longevity

In 2020, there were an estimated 727 million persons aged 65 years or over worldwide. This number is projected to more than double by 2050, reaching over 1.5 billion persons. By mid-century, one in six people globally will be aged 65 years or older. Globally, the population aged 65 years and over is growing faster […]
-
Sanford Stem Cell Symposium 2022

In late October of 2022, research and clinical experts from around the globe gathered for the Sanford Stem Cell Institute Symposium – a multidisciplinary event highlighting recent breakthroughs in regenerative medicine. Stakeholders from academia, industry, government, and the public discussed developments in the field for turning stem cell-based therapies into approved products for patients in […]
-
Preventing Heart Disease: What You and Your Doctor Can Do to Minimize Risk

What role do genetics, diet, exercise, and cholesterol play in preventing and treating diseases of the heart? In this program, you’ll learn about advances in the prevention and treatment of heart disease, and what you and your doctor can do to minimize risk with Dr. Carlin Long. This episode is part of a new series […]